By Bomb Cyclone The Bay Area was devastated by a “bomb-cyclone” storm with gale...
Blog
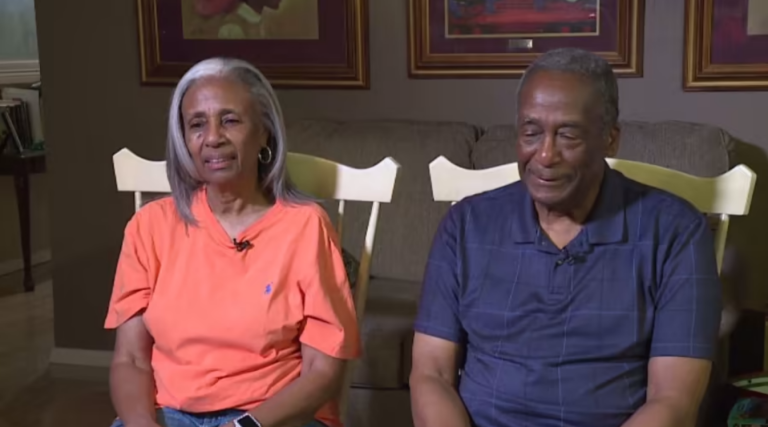
By Amy DavisA lot of Houston residents have seen the ads that say that...
BY ANIKA OSAKI EXUMOne suspect was captured on Sunday after an armed robbery took place...
A sturdy and secure roof is crucial for safeguarding your property from the elements....
Introduction: Toronto, the bustling metropolis with its diverse neighborhoods and stunning architectural heritage, provides...